Pre-analytical errors refer to the mistakes done while handling samples before they reach the actual testing paltforms.
Often, these are small slip‑ups but do the most damage to your lab’s reputation and credibility.
In many labs, around 70% of total errors are attributed to pre‑analytical phase—like a mislabeled tube, a missing form field, or a box that got too warm.
They kill your revenue and erode patient trust.
What’s the smart fix?
Use a digital tracking system such as a unique sample barcode so that every department knows which sample is which.
Let’s see how a digital sample tracking system prevents these pre-analytical errors.
Key Takeaways
- Pre‑analytical mistakes cause most lab errors but are preventable with the right systems.
- LIMS barcodes reduce clerical errors, boost traceability, and ensure compliance.
- Blending automation with best practices delivers reliable, fast, and safe lab results.
The True Cost of Pre-Analytical Errors
For a broader, operations‑friendly overview of common lab pitfalls across the entire testing lifecycle, see our companion guide, 10 Everyday Errors Costing Indian Labs Thousands. It pairs checklists with quick fixes you can roll out alongside the barcode steps in this article.
The Silent Killers: Haemolysis and Contamination
Pre‑analytical errors often start with the sample itself. Some common examples include:
- Haemolysis: Red blood cells break open, skewing test results. This may occur if the needle is too small, if blood is forced into a tube with too much pressure, or if the tube is shaken vigorously.
- Contamination: Occurs when the puncture site is touched after cleaning, or when poor disinfection practices are followed.
- Improper Storage/Temperature: Delays in transport or exposure to incorrect conditions can make samples unusable.
- Incomplete Documentation: Missing or incorrect forms often slow down processing and lead to repeat tests.
Both haemolysis and contamination remain among the most damaging issues, but small oversights in storage and paperwork add up to costly delays.
Avoiding Clerical Mistakes with Accurate Labeling
Clerical errors, such as misidentifying patients or mislabeling specimens, are common and can be fatal. Accurate patient-sample matching is a critical factor influencing the eventual laboratory result.
To ensure quality, labeling must be precise. The label should clearly include the patient’s full name, file number, date of birth, and the date and time of collection. This stringent process minimizes human error.
Upholding Sample Integrity Through Quality Control
Maintaining the integrity of the test sample is crucial across all stages: collection, handling, transportation, and processing. Quality assurance practices help minimize the chance of mishaps in the process.
The Importance of Temperature Monitoring
Temperature integrity is a major concern, particularly for distant testing scenarios. Most parameters remain stable at ambient temperature for only two to four hours after collection. Special packaging may be necessary if testing takes longer.
Always use electronic data loggers to monitor temperature during transit. If the temperature falls outside the recommended range, the lab must take corrective action, and the sample may not be accepted for testing.
Training and Ethical Practices
Invest in properly training your staff on policies, procedures, and hygiene. Clear training reduces exposure risks and prevents avoidable patient incidents.
Standards to follow: For step‑by‑step phlebotomy technique and evidence‑based pre‑analytical protocols, refer to the WHO Guidelines on Drawing Blood: Best Practices in Phlebotomy (NCBI Bookshelf). Use these as your baseline and let your LIMS barcode workflow document each step for audit‑ready compliance.
Implement Best Practices for Precision
Management must provide appropriate supplies, including single-use disposable needles and non-sterile, well-fitting gloves. Procurement should prioritize safety devices to reduce accidental injuries and blood exposure for staff.
Choose the Right System
Closed blood-sampling systems are generally safer than open systems because they reduce direct exposure to blood. Systems like vacuum extraction tubes make it easier to collect multiple samples during a single venepuncture.
For specific needs like arterial draws, specialized pre-heparinized syringes are required. The appropriate needle gauge must be used to prevent damage to the vein or blood cells (haemolysis).
Open vs. Closed Sampling Systems
| Feature | Open System (Needle & Syringe) | Closed System (Vacuum Tubes/Holder) |
|---|---|---|
| Exposure Risk | Higher risk; requires manual blood transfer to tubes. | Lower risk; eliminates blood transfer and splashing. |
| Multiple Samples | Difficult; requires transferring blood multiple times. | Easier; allows numerous samples from a single stick. |
| Cost | Generally the least expensive option. | Higher initial cost. |
| Skill Required | Requires user skill in transfer and filling. | Requires skill in use, especially with needle holder. |
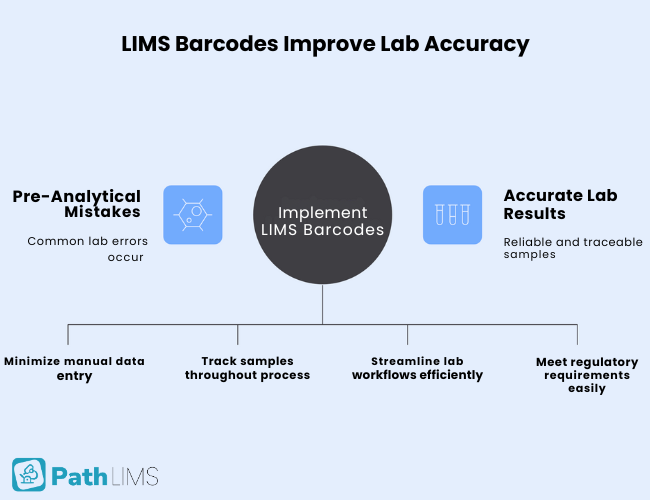
How LIMS Barcodes Solve Pre-Analytical Challenges
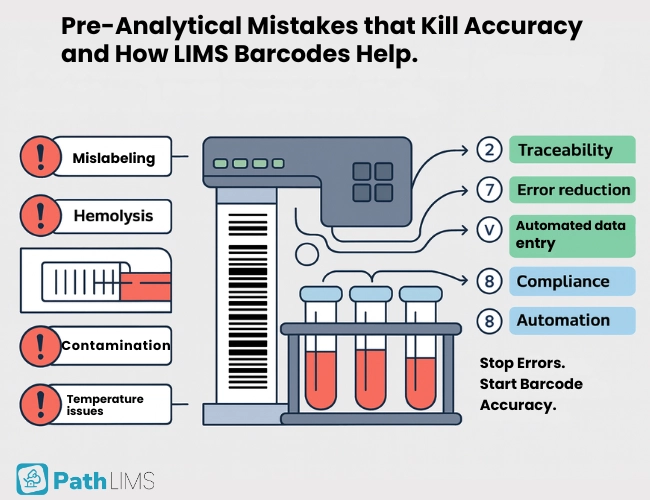
While best practices reduce risks, technology like LIMS barcoding makes error prevention systematic and scalable:
- Reduce Clerical Errors: Barcodes automate patient–sample matching, eliminating handwriting mistakes and misidentification.
- Improve Traceability: Each barcode carries a unique identifier, ensuring full chain-of-custody from collection to reporting.
- Automate Data Entry: Scanning barcodes integrates seamlessly with LIMS, reducing manual transcription and speeding up workflows.
- Support Compliance: Barcode-driven systems align with NABL and WHO standards for labeling, traceability, and quality assurance.
- Enhance Efficiency: Less time spent on relabeling or reprocessing samples means more reliable results delivered faster.
By embedding barcoding in every step of the pre-analytical process, labs can drastically reduce costly errors and ensure reliable, defensible data.
FAQs
How long can a sample last before being tested?
Many common parameters are stable for only two to four hours at ambient temperature (18° to 24°C) after collection. Others, like Glucose in plasma, are stable for six hours at room temperature, but several days when refrigerated.
What is the primary method to prevent contamination?
Health workers must practice rigorous hand hygiene before and after every procedure. They must clean the site with 70% alcohol and avoid touching it afterward.
Why is patient identification so important before drawing blood?
Accurate identification ensures the sample is correctly matched with the lab results, preventing clerical errors. Mislabeling can cause significant harm or fatal consequences due to misdiagnosis.
What safety procedures protect health workers?
Safety devices, such as retractable lancets, prevent injuries. Staff must avoid two-handed recapping and immediately dispose of sharps into a robust, puncture-resistant container within arm’s reach.
Wrapping Up
Accurate identification and sample integrity are the foundations of trustworthy results. Eliminating pre-analytical errors requires strict adherence to best practices in labeling, temperature control, and handling.
Integrating LIMS barcodes takes these safeguards further—minimizing clerical mistakes, boosting compliance, and protecting both patients and staff.PathLIMS helps you tackle all these issues—making your lab work faster, more reliable, and more accurate. Contact us today to discover how our solutions streamline operations and prevent costly mistakes.